Restricted Content
Please fill out the form below to access this content.
One out of every 13 people in the U.S. has asthma, and the majority of those affected are African-Americans, women, and children. The estimated yearly cost of this increasingly fatal condition is nearly $82 billion. These costs are in no small way negatively impacted by the highly variable controller medication adherence rate among asthma patients. In fact, as few as 30% of asthma patients use their asthma medications as prescribed. Cost impacts aside, improper medication adherence is clearly tied to an increase in the number of unplanned care episodes and heightened symptom severity. These medications are crucial to prevent and control asthmatic episodes, improve quality of life for those affected by asthma, and lower unplanned care costs for patients and health plans alike.
In 2010, Pennsylvania’s CHIP/Medicaid program had the fifth highest spend by state for asthma-related emergency department visits, spending nearly $13 million that year. One RxAnte health plan client did not accept this shocking statistic. They partnered with RxAnte to create a targeted CPP using telephonic intervention with Medicaid members receiving asthma controller medications. They asked the question: Can a clinical program with a predictive analytics foundation improve medication adherence and use, thereby improving patient wellness?
Program Design and Execution
The CPP pilot lasted eight months, from April through December 2017. Predictive analytics assessed data related to member demographics, pharmacy, and medical history, cross-referenced with medical and pharmacy claims data, to accurately identify the target population.
Predictive Model and Population Selection
The predictive model employed in the CPP used a combination of predicted adherence and eligibility in the HEDIS Medication Management for People with Asthma (MMA) measure. Patients ranged from 5 to 64 years old and were classified as having persistent asthma. Per the MMA measure, only those patients with prescribed controller medications who remained on those medications for at least 75% of their treatment period were selected for intervention. Ultimately, the population selected for outreach totaled 2,265 asthmatic patients at risk of non-adherence out of the 19,024 Medicaid members receiving controller medications in 2017. Baseline characteristics were subsequently established for those members targeted for outreach.
Contact and Intervention
Health plan pharmacists reached out to members via telephone and performed assessments regarding adherence to controller medication, inhaler technique, and proper medication use. Two attempts were made to reach each member for each session, and members received follow-up calls every four to six weeks.
Analysis
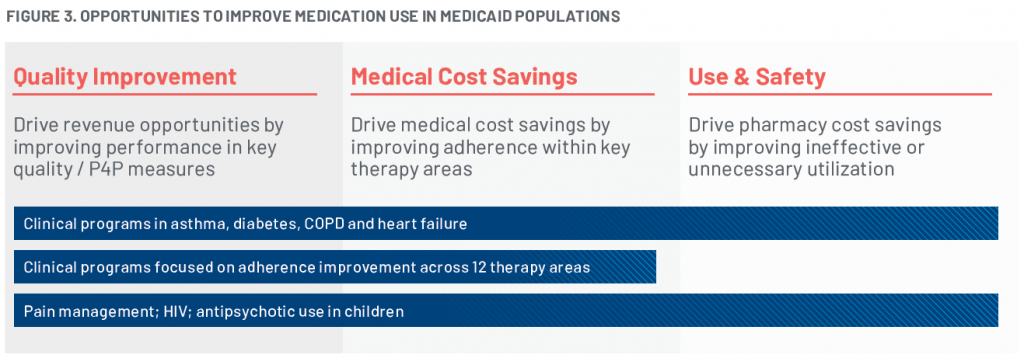
RxAnte’s assessment of adherence improvement— the primary outcome of interest— compared actual year-end adherence rates against the predicted baseline adherence prediction made at the initial selection date. This assessment applied to both the reached (receptive to clinical contact) and never reached (nonresponsive or nonreceptive to clinical contact) patient subsets. Secondary outcomes of interest included adherence barriers, rates of unplanned care, and condition severity.
Results and Adherence Lift
Nearly half of targeted members were reached, a quarter of which were assessed as having medium- or high-severity asthma. Year-end rates of adherence did improve compared to the baseline, most prominently among those who were receptive to clinical intervention. Estimated adherence improvement for members who had a discussion with a pharmacist versus those not reached was 8.6% (95% confidence interval), as illustrated in Figure 1.
As a result of barriers discussed during outreach, the identification of recent exacerbations in addition to other drug therapy problems will be added to the program going forward. Data also indicates that expanding this program to include other clinical measures, such as recent exacerbations or other drug therapy problems, may improve asthma-related outcomes.
The program uncovered several secondary outcomes, including a possible trend between intervention and reduction in unplanned care episodes (Figure 2), and common barriers to adherence. Forgetfulness (28%) and a lack of understanding of how to use controller medication (26%) were the two most commonly cited barriers to adherence; reached members also had a lower likelihood of a subsequent asthma-related unplanned care episode (2 per 1,000) versus those not reached.
At the end of the CPP, 44% of members had been reached, with an estimated 8.6% adherence improvement rate among those reached members and a significant population-level adherence lift of 6.8%.
Impacts on the Future of Healthcare
As trends across unplanned care episodes and receptivity to clinical intervention continues to be monitored, this program may have deeper clinical implications. Expansion of the CPP is now underway and will feature measures related to adherence, asthma exacerbation, therapy duplication and other indicators vital to cost and care quality management. CPP clinical intervention combined with RxAnte’s rich data legacy is blazing the trail for new, better healthcare and re-imagined strategies for improved medication use.
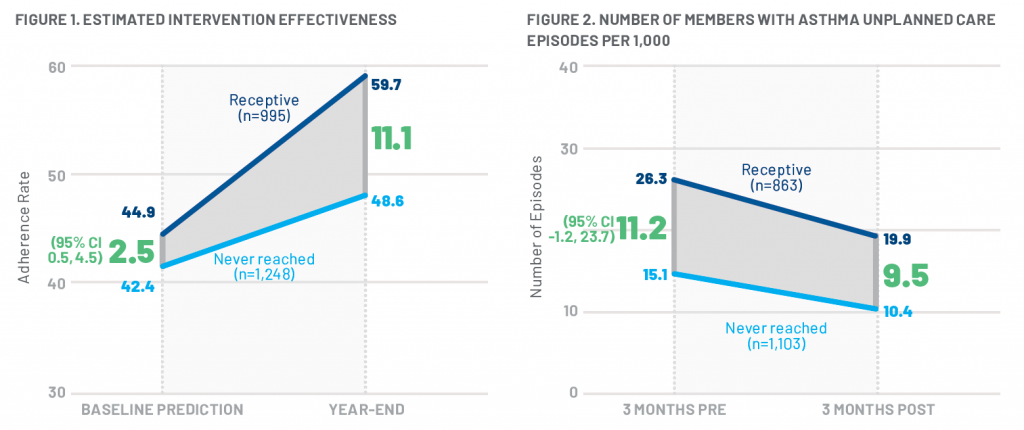
Looking ahead, RxAnte is engaging in additional opportunities to include medication use in Medicaid populations beyond the CPP program targeting asthma (Figure 3). Honing the ability to use predictive analytics to estimate adherence and performance measure eligibility among such key populations is a game-changer for medication adherence. Healthcare organizations and patients will both benefit from improved outcomes based on targeted, better informed interventions.