Background
Our regional health plan client identified a need to improve member adherence and optimize workflows. They believed a strategic medication adherence solution could support both their parent company and internal goals by realizing efficiencies in drug therapy programs, optimizing their member adherence strategy, and improving medication use. In late 2017, RxAnte partnered with the health plan to implement this solution in the form of RxAnte’s clinical workflow tool, RxEffect. This analytics and workflow platform is designed to bring scalability to pharmacy outreach and interventions. Customized to a health plan’s unique needs, RxEffect was designed to empower health plans to work more efficiently to provide higher-value care through more effective medication adherence programs.
Program Design and Execution
The RxEffect intervention program was first implemented in late 2017. Through this tool, health plan pharmacists organize outreach efforts directed at improving patient adherence for diabetes, RASA, and statins. The program is designed around these key performance drivers:
- Effective interventions that are collectively capable of achieving the required lift.
- Appropriate targeting directed at members most likely to benefit from interventions.
- Interventions deployed in a timely manner based on the target population.
- Scalable interventions spread over the entire pool of high-priority members.
Results for 2018 and Beyond
Analysis was restricted to therapies deployed with fills on or before the date of recommendation to ensure fair comparisons between the reached and not reached cohorts. RxAnte’s forecast provided a better metric for tracking to year-end performance than other leading retrospective reporting companies. It allowed us to see that the health plan continued a trend of year-over-year improvement in adherence rates throughout 2018 .
Impacts on Patient Fill Behavior
Pharmacists using RxEffect to conduct outreach have positive impact on patient fill behavior. Specifically, there are two important outcomes that relate to the program impact on member fill behavior – comparing reached and not reached member therapies attempted for outreach with fills due on or before the date of recommendations (to ensure fair comparison):
- Members who were due or late for medication refills and were reached filled their prescriptions an average of 4 days sooner than those not reached.
- 39% of members reached using RxEffect filled on the day they were reached. This is a nearly 5x improvement in same-day fill rates when compared to those members that were unable to be reached through RxEffect.
Enhanced Operational Efficiencies
RxEffect took on the role of identifying and prioritizing members for outreach and automated the health plan’s adherence program report-outs. This shouldered a moderate amount of the administrative burden typically required for this process. As a result, the plan has gained numerous efficiencies through RxEffect. This includes:
- Maximizing pharmacist time through predictive targeting of members most likely to benefit from a given intervention (versus previously utilizing lagging indicators that are unable to prioritize or indicate a member’s likelihood of adherence).
- Reallocating two FTEs to clinical activities following the removal of manual processes for program administration, reporting, and target list creation.
- Eliminating competing workflows, improving overall process management.
- Improving timeliness of outreach with dashboards that provided real-time monitoring and reporting.
Adherence for 2018 and Beyond
Our health plan client has benefited from member-level insights and administrative efficiencies through RxEffect, but how are the benefits of improved targeting, clinical outreach, and improved efficiency reflected at the population-level? Like many RxAnte clients, they remain on track for year-over-year improvements. They are forecasted to improve 2-3% in the three triple-weighted adherence measures in 2018. But we’re not stopping there.
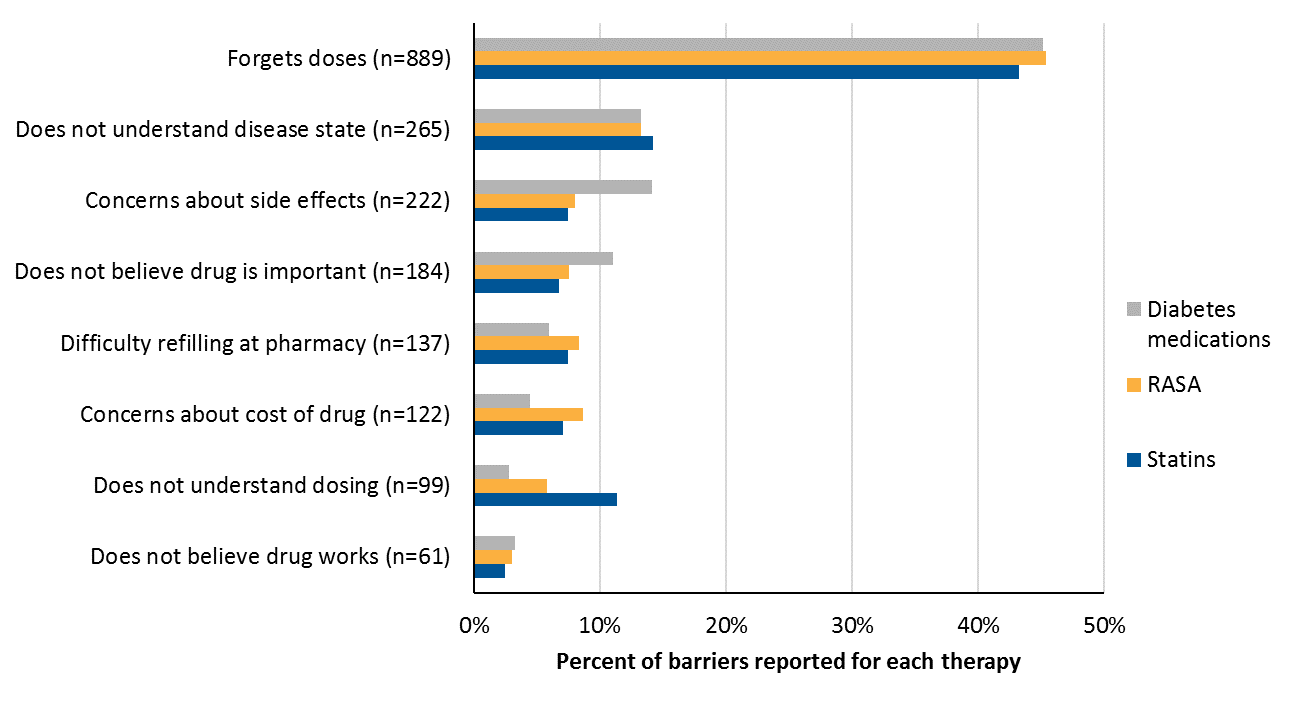
Taking the next step with medication adherence calls for identifying additional solutions or resources for patients based on common barriers to adherence, which can be captured via RxEffect. As we’ve found with this client and others, certain barriers cause adherence rates to decline, and those present an incredible opportunity to refine outreach strategies and methods. Working with our clients and through the barrier reporting in RxEffect, we’re able to refine adherence programs year after year to ensure that targeting is appropriate to each plans’ unique member makeup. The results continue to speak for themselves.
Impacts on the Future of Healthcare
Using RxEffect to orchestrate interventions, customized to a client’s needs and target population, brings a new level of measurement and depth to medication adherence programs. Health plans should consider adding cost-effective, scalable intervention elements, like interactive voice response systems, to drive population-level adherence lift; expanding the RxEffect platform to new measures and populations; and implementing the programs across regions.
RxAnte will continue to monitor the results of RxEffect and make customized improvements with this and other clients. We will explore other opportunities to enhance medication adherence with the platform as well, including the introduction of new modes of outreach to engage patients who are unreachable by phone, focusing on operational deployment, and exploring the effects of barrier resolution.
RxAnte can predict year-end adherence with 92% accuracy for a population of approximately 47,000 MAPD patients with at least one fill of a diabetes medication, RASA, or statin.
RxEffect isn’t the only way we can improve administrative efficiencies and patient outcomes. Let’s talk.