Restricted Content
Please fill out the form below to access this content.
Health plans face a complicated landscape today when it comes to medication adherence, but the goals remain the same: to improve access to care and optimize health outcomes. In our latest piece, we discuss the challenges of medication adherence for MAPD plans and their member populations; current approaches used to intervene and encourage better medication use; and how we might better reach and support vulnerable and medically complex Medicare members.
Attaining year-over-year improvement on triple-weighted Stars adherence measures remains difficult when faced with new quality measures, limited resources, and rising cut points. On top of these factors, health plans are challenged in helping those members who are the most medically complex and vulnerable. This segment of the population, containing Medicare members on multiple medications for chronic conditions, is at risk of non-adherence or is already non-adherent. Additionally, recent analysis shows that social determinants of health (SDOH) factors, including individuals’ economic, environmental, food, educational, and social situations, exacerbate existing challenges or create risks themselves. 1 With all of these concerns impacting health plans’ priorities today, how can payers encourage better medication use for this population?
What if Pharmacy Claims Data Could be Combined with Structured and Observational Data Collected in a Medically Complex Patient’s Home?
The industry standard in improving medication use leverages pharmacy claims data to identify members who are at the highest risk of becoming non-adherent, and then intervening with member outreach to encourage adherence. Most outreach involves live calls with the member as a reminder to refill medication and to help advise or resolve any barriers to adherence. While this method can be extremely valuable in resolving barriers like forgetfulness and confusion due to regimen complexity, the challenge lies in how to influence member behavior for the most vulnerable population.
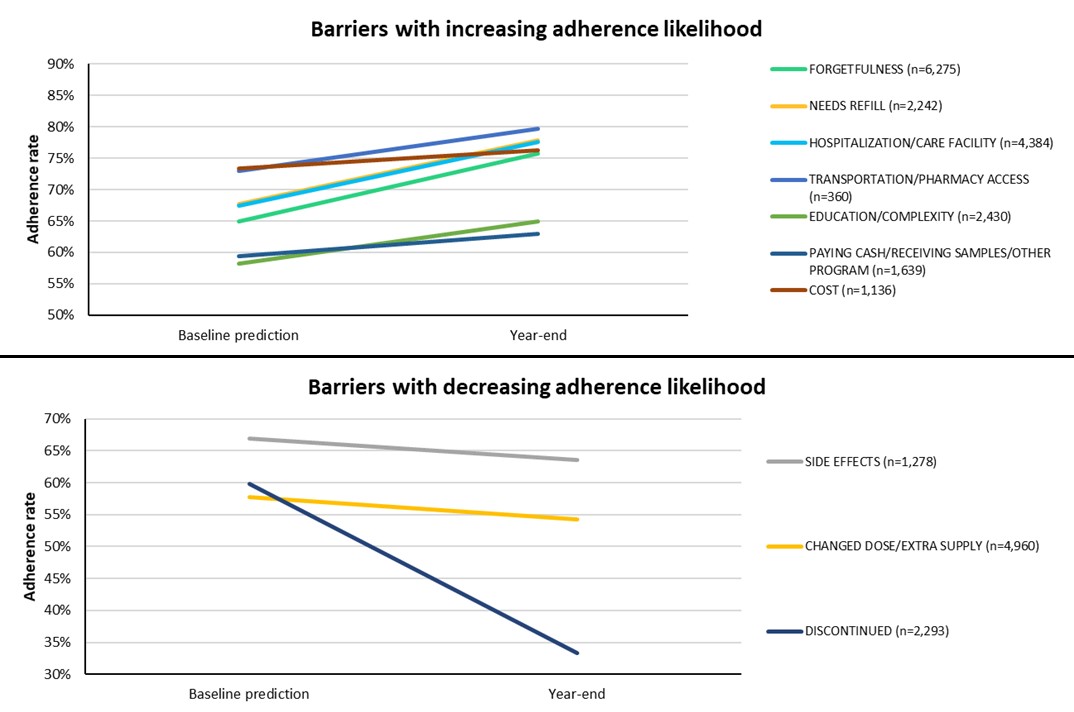
At RxAnte, we continue to see that the top-reported barriers for adherence—including unwanted side effects or change in dose— exist each year across health plans; thus while live outreach can identify these barriers, we often see variable success in resolving them (Figure 1). In the last year alone, RxAnte found that our health plan clients’ members who received outreach in the prior year still comprised 76 percent of non-adherent members by year-end. Thus, despite successfully contacting these high-risk members, the ability to actually influence plan member behavior for the more complex patients remains a significant challenge.
Figure 1
How Can Plans Successfully Engage Their Medically Complex and Vulnerable Members?
The medically complex and vulnerable population are referring to predominantly includes older adults, among the highest utilizers of health care services 2; nearly half of this population is taking one or more medications that are not medically necessary 3, and many members are prescribed a costly brand-name drug when a generic equivalent would be equally effective 4.
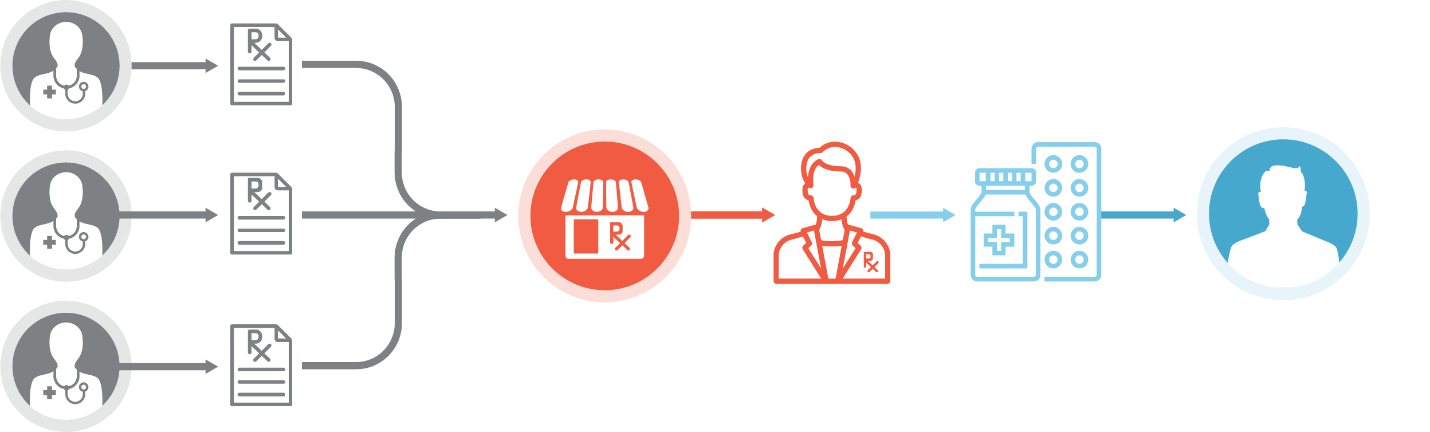
Under the traditional retail pharmacy model (Figure 2), the emphasis is placed on dispensing medications as indicated by individual scripts from prescribing physicians—there is no consolidated list of medications for a single member. Because of this narrow focus, the pharmacy lacks the ability to assess each member’s complete regimen for risks including, but not limited to: duplicate therapies, therapy gaps, drug-drug interactions, or other contraindications according to Beers criteria.
With traditional dispensing practices, there is limited to no opportunity to understand SDOH risks that create or intensify barriers to proper medication use, including cost and transportation challenges. We’ve seen this problem across the industry, and by enhancing the role of the pharmacy, we can improve the experience and outcomes for both the health plan and the member.
Figure 2
The Role of a Comprehensive Pharmacy Service
Research has shown that a pharmacists’ intervention can have a tremendous impact on the overall cost of care and member wellbeing, as demonstrated through reduced emergency visits and hospital readmissions. A recent study focused on a group of patients post-discharge, with just under one-third of the group receiving a discharge medicines review (DMR), and the rest receiving no review. Those patients receiving a DMR had a 45 percent chance of readmission in 90 days, versus a 56 percent chance for those who did not receive a DMR.5 Another study examining cost savings related to team-based care found that pharmacist-led interventions resulted in fewer hospital admissions and ED visits and an estimated savings of $3,697 per patient.6
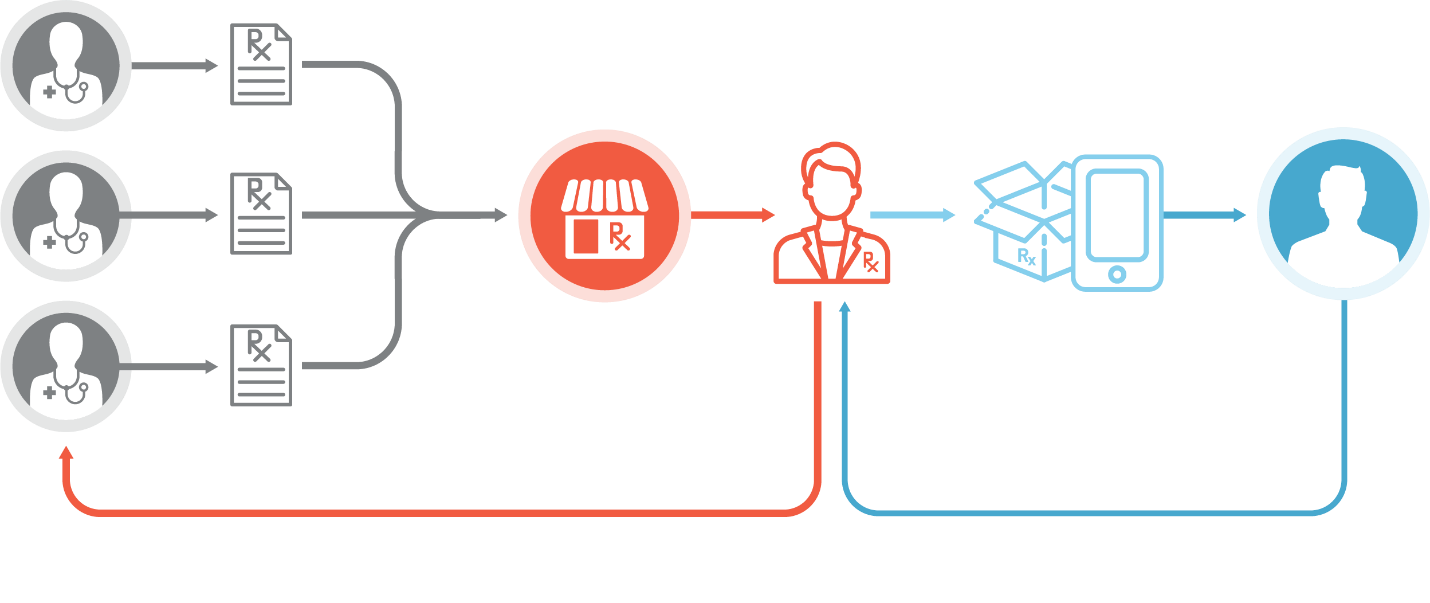
So how can we elevate the role of the pharmacist to realize these benefits on a larger scale? By equipping the pharmacist with the complete picture of each member’s regimen.
A comprehensive pharmacy service improves the care experience for complex and vulnerable members by accommodating feedback loops into the dispensing process. Once a member enrolls in the service, the pharmacist takes a central role in coordinating a consolidated medication list. Importantly, this is achieved by conducting a comprehensive medication review, with any recommended changes being conducted in conjunction with the member’s prescribers. From facilitating prior authorizations to optimizing regimens by accounting for cost, safety concerns, or unwanted side effects, the pharmacist is in a better position to help members achieve an ideal regimen (Figure 3). So what would this model look like once implemented?
Figure 3
Implementing a Comprehensive Pharmacy Service: Mosaic Pharmacy Service
Mosaic Pharmacy Service is a comprehensive pharmacy service backed by RxAnte analytics to resolve adherence barriers and address key factors affecting proper medication use. By combining analytics-enabled care management, in-home care, and medication delivery, Mosaic has established a transformative pharmacy experience for health plans and their members. A combination of regimen optimization and attention to social determinants of health challenges managed by Mosaic’s clinical pharmacists make this the most powerful intervention designed to improve medication use for the medically complex and vulnerable members it serves.
Eligible members are offered the service through multiple referral channels, including their health plan or long-term care facility. For home-based patients, the enrollment process consists of a home visit, which features a medication use review and data collection to identify social determinants of health risks. Research supports the critical impact that home visits have on this medically-complex segment of the population, with recent studies citing benefits including regimen simplification and reduction in non-heart failure hospital days attributable to a pharmacist’s home visit. 7
A clinical pharmacist then completes a comprehensive medication review to ensure the member is on their ideal regimen, advising on methods to optimize prescriptions that are agreed upon together with the prescribing physician. By collaborating directly with the member’s prescribing physicians and health plan, Mosaic syncs all medications into the safest, simplest regimen that is delivered in easy-to-use packaging to encourage adherence and proper use. According to a recent study published in Health Affairs, patients are more likely to have have improved adherence particularly those who take cardiovascular medications when participating in medication synchronization programs. 8
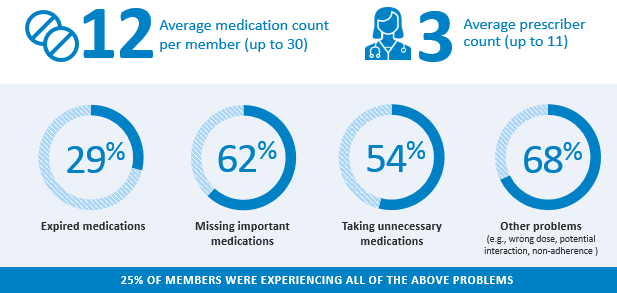
With its unique care model, Mosaic has uncovered and intervened to address critical medication problems such expired or unnecessary medications for 90% of its members (Figure 4). Powerful results are already emerging from patient stories and provider testimonials as the pharmacy resolves issues related to cost, confusion, safety, and regimen complexity.
Figure 4
As the pharmacists’ role continues to evolve and add enormous value in the ability to influence positive change for the most medically complex and vulnerable population, it’s important to ensure that health plans utilize a comprehensive pharmacy service to encourage better medication adherence and address the most pressing social determinant of health factors that face this segment of our communities.
REFERENCES
1. Patel, Minal R et al. “Social Determinants of Health, Cost-related Nonadherence, and Cost-reducing Behaviors Among Adults With Diabetes: Findings From the National Health Interview Survey.” Medical care vol. 54,8 (2016): 796-803.
2. Zayas, Cilia E et al. “Examining Healthcare Utilization Patterns of Elderly Middle-Aged Adults in the United States.” Proceedings of the … International Florida AI Research Society Conference. Florida AI Research Symposium vol. 2016 (2016): 361-366.
3. Nechba, Rhita B et al. “Difficulty in managing polypharmacy in the elderly: Case report and review of the literature.” Journal of Clinical Gerontology and Geriatrics. vol 6(2015): 30-3.
4. “White Paper: Sidelined: How Seniors Miss Out On Savings Available Through Generic Substitution.” Association for Accessible Medications. Retrieved by https://accessiblemeds.org/resources/reports/AAM-white-paper-seniors-sidelined-generic-substitution
5.Burns, Corrinne. “Pharmacist-led medication reviews after hospital discharge significantly cut chances of readmission.” The Pharmaceutical Journal (February 2020)
6.”Exploring Pharmacists’ Role in a Changing Healthcare Environment.” Avalere Health (2014). Retrieved by https://www.nacds.org/pdfs/comm/2014/pharmacist-role.pdf
7. Ely, Kaitlynn. “Study Shows the Impact Synchronization Programs Have on Medication Adherence.” AJMC. (2018).
