In our whitepaper Trends in Medicare, we wrote:
“It should come as no surprise that some of the most researched aspects of healthcare relate to chronic conditions such as heart disease and diabetes. Despite a wide array of drugs that exist to treat and manage these conditions, they remain among the leading causes of death in the nation. They are also among the top six leading causes of death among seniors.”
We find our MAPD clients often miss this opportunity to treat this subset of the population differently – and it is, indeed, an opportunity. 78 million U.S. residents will be seniors (65-years old and older) in the next twelve years. Three out of four seniors have multiple chronic conditions. It’s clear that understanding the ins and outs of these members is not only useful, it’s critical.
In fact, we find that there is measurable value in targeting medication adherence programs at seniors with chronic conditions. With more customized outreach and tailored interventions, medication adherence can improve far more than drug efficacy for this population. To get there, it takes clearer organization of the current data and better methods of capturing and reviewing new data going forward.
Chronic Conditions, Costs, and Adherence
The link between chronic conditions, medication adherence and total cost of care are well-documented, but the problem is still complex – see below:
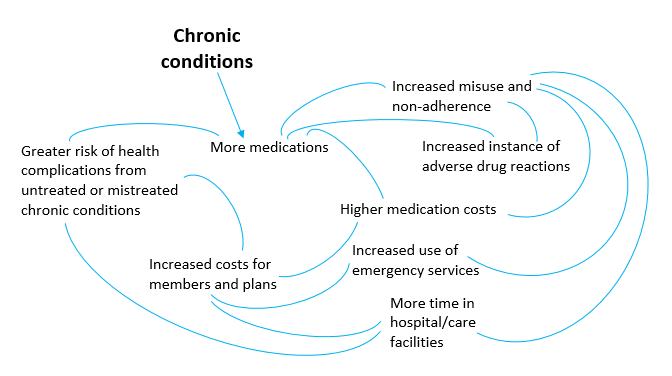
The element of age only amplifies these complications. Understanding that, and understanding this intricate cycle gives health plans the opportunity to break it. They can step in at critical moments, shifting the narrative away from over-prescribing and toward a system of managing health and wellness.
How MAPD Plans Break the Medication Non-Adherence Cycle
The health plan is often best positioned to deploy solutions that aim to improve member health and subsequently reduce cost of care. We know that the most effective adherence programs employ a portfolio of interventions (such as email, SMS, and automated and live calls) that are deployed at the right moment to effect member behavior before habitual non-adherence sets in. The recipe for achieving this successfully includes:
- A members based upon risk of medication-non adherence and urgency
- Targeted, precisely timed, and scalable interventions.
- The ability to capture and analyze intervention outcomes in order to improve prediction models and member targeting
See how RxAnte’s solution is designed to achieve these objectives here.
Improving Your In-flight Adherence Program Using Outcomes Data
Consider our own case study analyzing the Medicare population of a large regional health plan client. It revealed that members adherent to cardiovascular prescriptions are .89-2.76 percent less likely to undergo cardiovascular procedures. Seemingly small improvements to the adherence rates of members with diabetic and cardiovascular treatments literally net thousands of dollars in annual, per member savings for plans. What do health plans like this one do differently to generate these savings? Learn from their interventions.
At RxAnte, there is one thing we know that no medication adherence program – targeting seniors or otherwise – can be successful without: capturing intervention outcomes to inform future program tactics. It’s common to find technology and platforms in this space that gather massive amounts of data and sometimes support interpretations from that data. It’s less common to find owners of that data who have the time or resources to take actions based on those interpretations. For MAPD plans looking to tackle senior care in a cost-rewarding and competitive way, that’s critical. These plans must deploy solutions that include the ability to capture intervention outcomes and identify and resolve members’ barriers to medication adherence at the individual level. This approach makes actionable, evidence-driven insights truly valuable in breaking the medication non-adherence cycle among senior populations.
Part D plans: Learn more about our perspectives on MAPD populations and adherence in our full whitepaper – access it here.